
The ankle and foot work together to provide support, shock absorption, balance, and other functions essential for movement. While most minor injuries heal on their own, severe injuries and chronic conditions should be evaluated by an orthopaedic specialist. Call WRMC Orthopaedic and Sports Medicine Clinic at (870) 793-2371 for an appointment.
Ankle Injuries
Foot Injuries
The hand and wrist are a complex set of bones, joints, ligaments, muscles, and tendons. Overuse injuries may cause pain and stiffness, limiting the ability to complete activities of daily living, enjoy hobbies and sports, and work. Pain and stiffness that limit function and last for more than two weeks should be evaluated by an Orthopaedic Specialist. To make an appointment with one of our providers call, (870) 793-2371.
Hand and Wrist Conditions
Hand and Wrist Treatments
Hip and or knee pain that limits the ability to walk and limits your daily activity should be evaluated by an Orthopaedic specialist. Constant, debilitating joint pain is not a normal part of the aging process. Pain may be caused by arthritis, sport injuries, trauma, or work-related injuries, and may worsen over tie if the underlying cause of the pain is not addressed.
Our surgeons have extensive training and experience in the diagnosis and treatment of hip and knee conditions. We will diagnose the cause of your pain and work with you to develop an effective treatment plan.
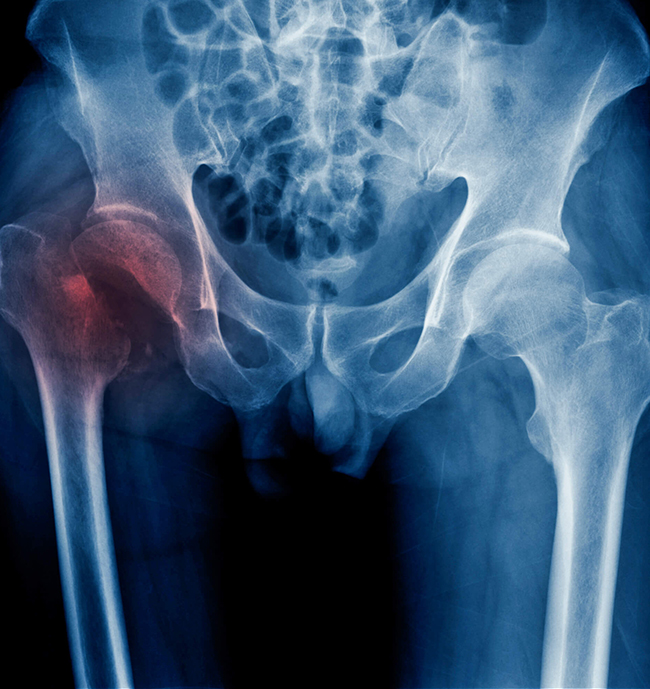
Hip Conditions and Treatments
Minimally Invasive Direct Anterior Approach Hip Replacement
Direct anterior approach is a minimally invasive surgical technique for total hip replacement. Patients undergoing and anterior approach hip replacement generally have a shorter hospital stay, lower pain, and quicker return to regular activities.
Direct anterior approach is a minimally invasive surgical technique for total hip replacement. Patients undergoing and anterior approach hip replacement generally have a shorter hospital stay, lower pain, and quicker return to regular activities.
Robotic Assisted Hip Replacement
Using Mako® robotic assisted surgical technology, surgeons provide hip replacement surgery personalized to each patient’s diagnosis and unique anatomy. Before surgery surgeons use a CT scan of the hip to create a 3D virtual model of the hip and the Mako software to develop a pre-operative plan. During surgery, the surgeon guides the Mako® robotic arm to remove the arthritic bone and insert the hip implant.

Knee Conditions and Treatments
Knee pain may be resolved with conservative therapies such as rest, bracing, and physical therapy. When conservative treatments are unsuccessful, an Orthopaedic specialist may recommend injections or surgical intervention.
Robotic-Assisted Partial and Total Knee Replacement
Using Mako® robotic assisted surgical technology, surgeons provide partial and total knee replacement personalized to each patient’s diagnosis and unique anatomy. Before surgery surgeons use a CT scan of the knee to create a 3D virtual model of the hip and the Mako software to develop a pre-operative plan. During surgery, the surgeon guides the Mako® robotic arm to remove the diseased joint and prepare the bone for placement of the knee implant. The Mako® system allows the surgeon to adjustments to the plan as needed during surgery to ensure an accurate placement of the implant.
Shoulder and elbow pain may be caused by arthritis, injury, or repetitive motion during sports or work activities. The physicians of WRMC Orthopaedic and Sports Medicine Clinic are experienced in the diagnosis and treatment of upper extremity conditions. Our goal is to provide treatment that relieves pain, restores function, and allows patients to resume an active and healthy lifestyle.

Shoulder Conditions and Treatments
Elbow pain is usually an overuse injury caused by repetitive motion and stress to the joint. These injuries are most common in golfers, pitchers, and athletes playing racket sports. Our orthopaedic specialists evaluate patients with elbow pain and may prescribe conservative treatments such as anti-inflammatory medication to relieve pain, rest, bracing, physical therapy, and at home exercise. Conditions that don’t respond to conservative treatment may require a surgical intervention.

Common Elbow Conditions and Treatments
What is Osteoarthritis?
Osteoarthritis is the most common form of arthritis. It is also called degenerative joint disease or wear and tear arthritis. It occurs more frequently in the hands, hips, and knees.
With osteoarthritis, the cartilage within a joint begins to break down and the underlying bones begins to change. These changes usually develop slowly and get worse over time. Osteoarthritis can cause pain, stiffness, and swelling. In come cases, it limits function and causes disability; some people are no longer able to do daily tasks or work.
What are the Signs and Symptoms of Osteoarthritis
How Many People Have Osteoarthritis?
Osteoarthritis affects more than 30 million US adults.
What Causes Osteoarthritis?
Osteoarthritis is caused by damage or breakdown of joint cartilage between bones.
What are Risk Factors for Osteoarthritis
How is Osteoarthritis Diagnosed
A doctor diagnoses osteoarthritis through a review of symptoms, physical examination, x-rays, and lab tests.
How is Osteoarthritis Treated
There is no cure for osteoarthritis, doctors treat osteoarthritis symptoms with a combination of therapies, which may include the following:
In addition to these treatments, people can gain confidence in managing their osteoarthritis with self-management strategies. These strategies help reduce pain and disability so people with osteoarthritis can purse the activities that are important to them. These five simple and effective arthritis management strategies can help.
How Can I Manage Osteoarthritis and Improve My Quality of Life
The Centers for Disease Arthritis program recommends five self-management strategies for managing arthritis and its symptoms.
Learn More about Osteoarthritis
Learn More about Arthritis
Content provided and maintained by the US Centers for Disease Control and Prevention. (CDC) Please see our system usage guide and disclaimer.
Accidental or sports injury, prolonged stress from overuse, and osteoporosis are the most common causes of orthopaedic fractures. If you experience symptoms associated with a fracture, it is important to seek emergency medical treatment. WRMC Orthopaedic and Sports Medicine Clinic Surgeons provide orthopaedic trauma care at White River Medical Center’s Emergency Department. If you experience a medical emergency call 911.
Symptoms
X-rays or CT scans are usually used to confirm diagnosis and show the type and exact location of a fracture. Casts and splints may be used to treat simple or stress fractures. Complex fractures may require surgery to reposition the broken bone for proper healing and may require plates and screws to stabilize the bone during healing.
Types of Fractures
The following general terms are used to describe most fractures
Joint replacement surgery removes damaged or diseased parts of a joint and replaces them with a joint implant. Our surgeons offer Hip, Knee, and Shoulder replacement surgery.
Joint replacement surgery may be recommended after more conservative treatments, such as lifestyle changes, physical therapy, and medication, are unsuccessful. It may also be recommended if pain limits and restricts mobility, making routine activities difficult.
Our approach to joint replacement surgery recognizes that our patients and their support system are important members of the care team. The White River Medical Center Orthopaedic Liaison and our staff work with each patient to coordinate education, surgical pre-admission testing, and insurance pre-certification necessary to prepare for surgery. Our goal is to improve mobility, relieve pain, and restore function for every patient allowing them to return to a healthy, active life after surgery.
Joint Replacement Services Offered
Robotic Assisted Joint Replacement
Our surgeons use robotic assisted technology for partial knee, total knee, and total hip replacement surgery. Using the Mako® Robotic Assisted Surgical system, surgeons create a personalized surgical plan based on each patient’s unique anatomy. Clinical studies comparing Mako® Robotic Assisted Surgery to conventional joint replacement report the following:improvements in the fit and anatomical alignment of the prosthetic joint, reduced soft issue injury, lower pain scores, and higher satisfaction.
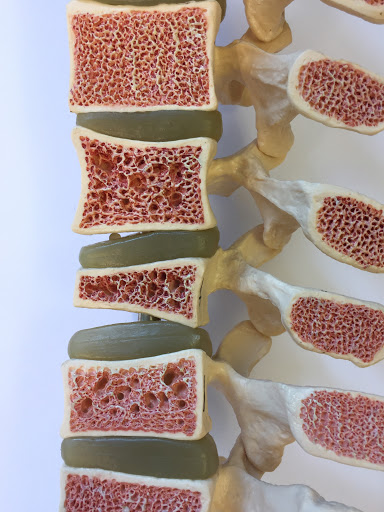
Risk Factors You Can't Change
Some risk factors for osteoporosis cannot be changed. These include
Risk Factors You Can Change
There are other risk factors for osteoporosis that can be changed.
The good news is that it is never too late to improve your bone health. Work with your provider to evaluate your risk factors, pay careful attention to warning signs, and take steps to maintain healthy bones.
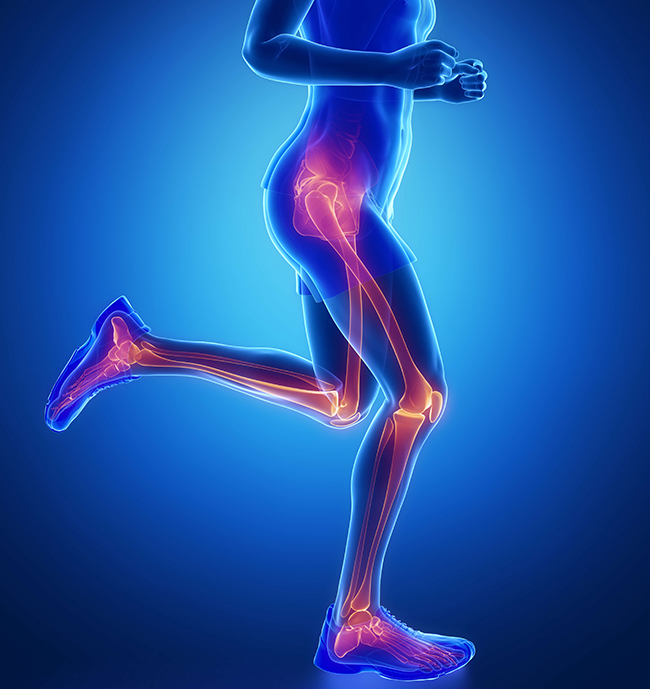
The Orthopaedic Specialists at WRMC Orthopaedic and Sports Medicine Clinic provide diagnosis, treatment, rehabilitation, and injury prevention recommendations for athletes and fitness enthusiasts at every age and skill level. Physicians may also provide consultation to athletes for agility, endurance, and strength training. Our team includes an American Academy of Orthopaedic Surgeons certified Sports Medicine Specialist and fellowship trained Sports Medicine Specialist. Orthopaedic Surgeons are on call to ensure access to timely care in the event of an orthopaedic sports injury. Call our clinic at (870) 793-2371 to learn more about our Sports Medicine services.
Common Sports Injuries
When an orthopaedic injury occurs at work it is important to seek prompt treatment. Our clinic is dedicated to providing efficient patient centered care to treat many work-related injuries and help patients return to work as soon as safely possible. We work closely with human resource departments to ensure proper documentation to satisfy worker’s compensation insurance requirements. If you are injured at work, call (870) 793-2371 to discuss an evaluation.
Common Orthopaedic Work Injuries
Note - WRMC Orthopaedic and Sports Medicine Clinic is a general Orthopaedic practice and we do not treat diseases or injuries of the back and spine.
Arthroscopy is an outpatient surgical procedure used to visualize, diagnose, and treat conditions inside the joint. During an arthroscopic procedure, the surgeon inserts an instrument with a camera and light into a small incision. Images are transferred onto a screen to allow the surgeon to see inside the joint and confirm diagnoses. Instruments may be inserted through other small incisions to allow the surgeon to repair cartilage, ligament, or tendon damage.
Arthroscopy is minimally invasive and most patients report less pain and quicker return to daily activities when compared to open surgery. Most patients return to work or school in a few days. It is important for patients to follow post-operative instructions carefully to prevent complications and allow healing.
Arthroscopic Procedures
The Orthopaedic Surgeon may recommend injections to relieve joint pain and inflammation as a part of an overall plan of care. Injections may be recommended in conjunction with other treatments before surgical intervention is considered. Relief is usually felt within a few days following the injection and may last up to six months. Injections are effective in the temporary relief of pain and inflammation.